 What Do They Mean? Mild PAH?
What Do They Mean? Mild PAH?
We receive many emails from our readers inquiring whether having borderline to minimally elevated echo estimated pulmonary artery pressures means that they have pulmonary arterial hypertension. This is a very important question and many doctors unfortunately don’t understand the limits of echocardiography so patients are often left more confused.
Let’s review some of the basics to start.
- The diagnosis of pulmonary arterial hypertension is never made by echocardiography. The pressures that are reported are estimated and the echo is not able to give a clear picture of the left sided pressures, the blood flows and the resistance in the pulmonary arteries.
- The upper limit of normal for estimated pressures depends on how old you are, at what elevation you live and your other medical issues.
- If the diagnosis of PAH is being seriously considered, right heart catheterization is a necessary test.
What Do I Look For?
When I am asked to see a patient with minimally elevated echo estimated pressures I start by taking a history and examining the patient. Are there symptoms of shortness of breath? Is there a pattern of decreasing exercise capacity? Are there other disease processes present that make PAH more likely? Is there a history of diet pill use, stimulant use, prior episodes of blood clots, obstructive sleep apnea, diabetes? Is there a family history of PAH?
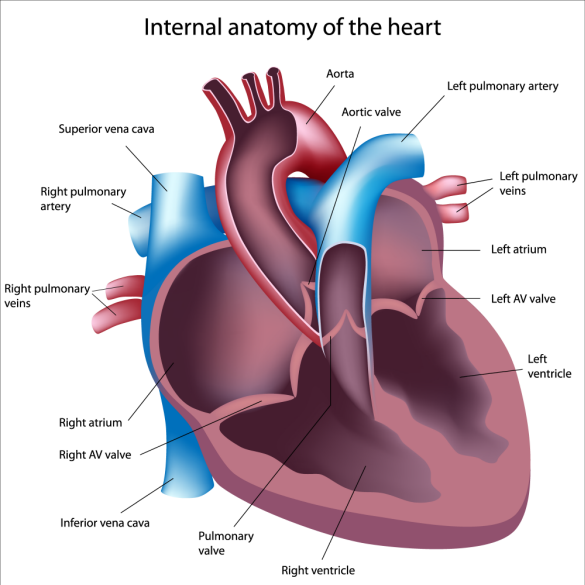
On physical exam I look for any abnormalities in heart, lung, skin, joints. Next I look at the available data, especially the echocardiogram, chest imaging and pulmonary function tests. On the echocardiogram I look to see if the right ventricle is normal in size and function? Is the left ventricle normal in size and systolic and diastolic function (does the left ventricle squeeze and relax normally)? Is the left atrium enlarged? How did the echo reader come to calculate the pulmonary arterial pressure? What assumptions were made?
After all of that I am usually able to decide if there is a high or low probability that that the patient has PAH or not. If all of the data argue against PAH then I often will repeat an echocardiogram in a few months. If there is enough to make me worry about PAH then I generally move forward and perform a right heart catheterization.
Patients with advanced lung disease often have mildly elevated pulmonary artery pressures and this is a different disease than PAH. Patients with left heart problems also often have minimally elevated pulmonary artery pressures and this is also not PAH.
Lastly, don’t panic if you had an echocardiogram that was read as showing minimally elevated pressures. Out of every 10 new patients that I evaluate for possible PAH, 7 don’t have PAH. They have another problem to explain their symptoms or echocardiogram findings. It is important not to jump to conclusions. Simply because an echocardiogram or CT scan of your chest has a report that includes the words Pulmonary Hypertension does not mean that you have PAH. Start by scheduling an appointment with your doctor to review the findings. If you remain worried then try and see a PAH specialist.
