 Disease Overview
Disease Overview
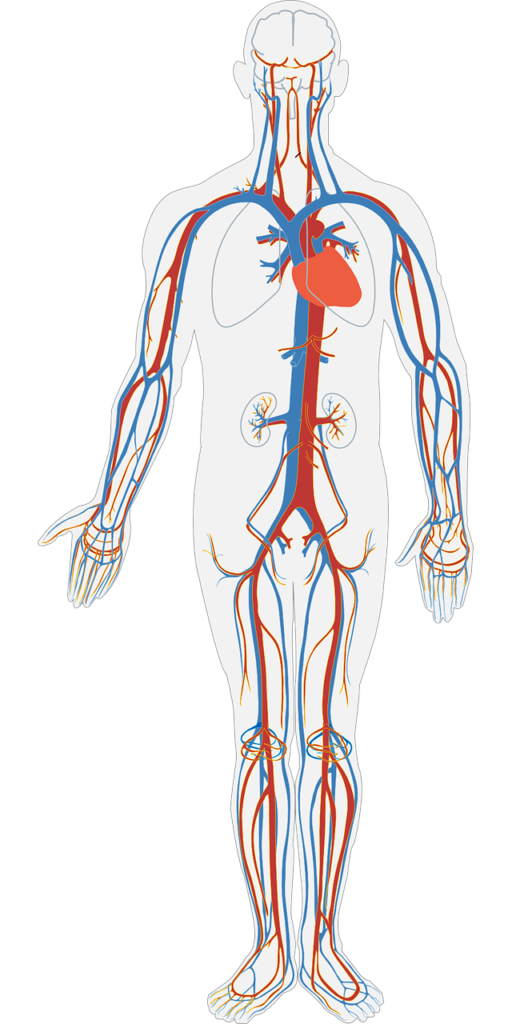
HHT is a rare disease that leads to abnormal blood vessel growth throughout the body. This commonly leads to frequent nose bleeds (epistaxis), gastro-intestinal bleeding and anemia. The more serious manifestations include abnormal blood vessels in the lungs, brain and liver. These abnormal blood vessels can lead to infections in the brain, bleeding in the brain, liver failure and pulmonary arterial hypertension.
Who gets HHT?
HHT is a genetic disorder that is inherited from your parent. It is autosomal dominant. This means that if one of your parents has the disease there is a 50% chance that each child will develop the disease. About 1 in 5000 to 8000 people are affected by the disease. This means that there are about 50,000-100,000 affected people in the United States. All races and ethnicities are affected by HHT.
What causes HHT?
There are three common genes that have been identified that lead to HHT. Mutations in Endoglin lead to HHT1. Mutations in ALK-1 lead to HHT2. Mutations in SMAD4 lead to juvenile polyposis-HHT (JPHT) overlap syndrome. Although earlier work suggested that HHT1 and HHT2 patients had different disease manifestations, recent work suggests that this may not be the case. The mutations in the genes that lead to HHT cause abnormal signaling by affecting TGF-Beta proteins.
Clinical Manifestations
Telangiectasias is the most common manifestation seen in all patients with HHT. These are tiny red dots or lines that most commonly develop on the lips, face, chest, fingertips. These are small abnormal blood vessels that are just under the skin or mucous membranes (mouth, nose or gastro-intestinal tract). These abnormal blood vessels are prone to bleeding. This leads to the most common symptom in HHT—nose bleeds. Almost all patients with HHT experience nose bleeds starting at an early age. It is important to remember that nose bleeds are common in the absence of HHT so the vast majority of people that have nose bleeds do not have HHT.
Arteriovenous malformations (AVMs) are larger blood vessels that form abnormally and connect the artery to a vein. These range from very small in size to very large. They commonly develop in the gastrointestinal tract, lungs, liver and brain. Although these abnormal blood vessels are less common than telangiectasias, they can cause life threatening problems.
- Pulmonary AVMs can lead to stroke and brain abscess when particulates or bacteria travel to the brain bypassing the filtering system in the lungs. If pulmonary AVMs rupture (pop) this can lead to life-threatening bleeding. Low oxygen levels are commonly associated with these abnormal blood vessels in the lungs. As blood bypasses the proper circulation, blood without oxygen is mixed with oxygenated blood (shunting). The net result is lower oxygen levels. Some patients will notice shortness of breath. In large pulmonary AVMs, the right side of the heart has to work extra hard and this may lead to right heart failure.
- Gastrointestinal (Bowel) AVMs may bleed. This is recognized by passing large amounts of red, maroon or dark blood in your stool.
- Brain AVMs represent a particular challenge. These abnormal vessels are prone to bleeding.
- Liver AVMs can lead to slowly progressive confusion and eventually liver failure.
Aneurysms in blood vessels of the brain may also be seen in about 10% of HHT patients. These abnormal outpouchings of the vessels are more likely to bleed leading to a type of stroke called subarachnoid hemorrhage.
Iron deficiency anemia is very common in HHT patients.
Pulmonary Arterial Hypertension with HHT
Pulmonary arterial hypertension develops in about 10-15% of patients with HHT. These patients will notice increasing shortness of breath as the most common symptom. The disease is indistinguishable from idiopathic pulmonary arterial hypertension in symptoms.
Migraine headache and blood clots are more common in patients with HHT.
How do we make the diagnosis of HHT?
There was an international meeting years ago in Curacao that resulted in an agreement on how we make the diagnosis of HHT. Four criteria were identified including frequent nose bleeds, multiple telangiectasias, abnormal blood vessels in the lungs/liver/brain/GI tract, and a family member with HHT. Each of these is given one point.
- Definite disease: at least 3 of the 4 criteria
- Suspected disease: 2 criteria
- Unlikely: 1 criteria
Genetic testing is available but not required to make the diagnosis. Identifying a mutation in the genes that cause HHT confirms the diagnosis. However, many patients will have mutations that are not able to be identified at this time.
Arteriovenous Malformations (AVMs) are identified by CT scanning or angiography of the lungs, abdomen, or brain.
Pulmonary hypertension is often suggested by an abnormal echocardiogram and then confirmed with right heart catheterization.
For information about the treatment of HHT click here.
