We had a wonderful topic suggestion from a reader. Essentially, how does one tell if they have Pulmonary Arterial Hypertension if there are conflicting tests? A common scenario goes something like this:
The echocardiogram shows no pulmonary hypertension but a CT scan shows pulmonary hypertension. A cardiologist repeats an echo that shows no pulmonary hypertension.
Is it possible to have pulmonary hypertension without pulmonary hypertension?
The question gets at a key issue in PAH—how do we make the diagnosis? There are a variety of tests that can suggest pulmonary hypertension and even PAH. However, there is only a single test that can confirm the diagnosis of PAH.
- CT scanning uses xrays to create an accurate image of your chest. When done with contrast we can measure the size of your pulmonary arteries quite precisely. When the pulmonary arteries are enlarged the radiologist interpreting the scan will often report “findings suggestive of pulmonary hypertension”. A less careful radiologist will just report “pulmonary hypertension by CT criteria”. The problem is that enlarged pulmonary arteries can be seen with many diseases and most are not actually PAH.
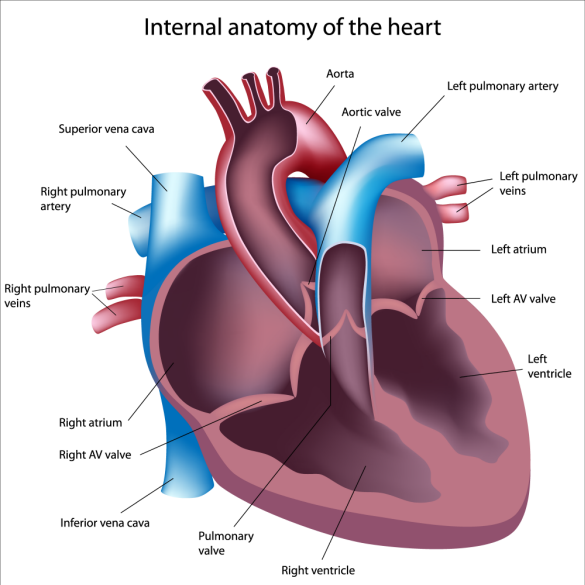
- Echocardiography is helpful in suggesting PAH. We can estimate the pressure in the pulmonary arteries and can evaluate the size and function of the chambers and valves in your heart. However, the pressure estimates are often not accurate and many echo labs don’t report the diastolic function of the heart (the relaxation phase of the heart muscle).
- EKG records the electrical activity of the heart and can be suggestive of PAH.
- Chest Xray can also suggest pulmonary hypertension by showing enlarged pulmonary arteries and a normal left side of the heart.
Right Heart Catheterization
The above tests though helpful do not provide enough information to confirm the diagnosis of PAH. A right heart catheterization is required. This test directly measures the pressure in the right side of the heart and the pressure reflected back from the left side of the heart. Blood flow is measured as well.
So how can two tests give different answers? Getting the most information from the echo report requires more than just the estimated pulmonary artery pressure. The size and function of the ventricles and the valves are very important. For example, a patient with normal right ventricle size and function but left ventricular dysfunction may have mildly elevated estimated pulmonary artery pressures that are explained by left heart problems. In contrast, a patient with a very dilated right ventricle but normal estimated pulmonary artery pressure who is short of breath requires a right heart catheterization to exclude PAH.
To make a determination, the following needs to be known.
- Why were the echo and CT scans done in the first place?
- Was everything else ok on the echo? Specifically, was the right ventricle normal in size and function? Was the left ventricle normal? Were the valves normal?
The most likely scenario is there is not PAH present. But without more information there is no way to be sure. If your cardiologist is pointing their finger at the pulmonologist and the pulmonologist is pointing their finger at the cardiologist you are in good company. Most of my patients are stuck in the middle of this finger pointing. Find a doctor expert in PAH and seek an opinion.
