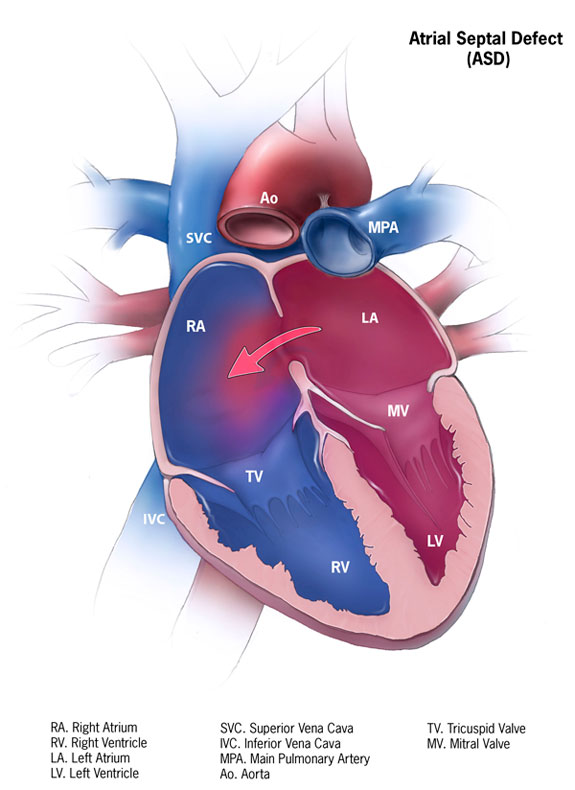
An Atrial Septal Defect (ASD) is a hole in the heart between the right and left top chambers (atria). This is not terribly uncommon with an estimated 1-2 per 1000 live births. Most of these holes are small and do not cause long-term problems. In some patients the hole is larger and can lead to extra blood flowing from the left side of the heart into the right side of the heart. Over time this leads to the right ventricle having to do extra work and the pulmonary arteries carry extra blood flow.
Changes in the Heart
The first changes that we see are that the right side of the heart begins to enlarge. Then the pulmonary artery pressure begins to increase. At this time many patients will start to notice that they are tired or short of breath. If you check your oxygen saturation during vigorous exercise you may find that your oxygen saturation drops. At rest your oxygen saturation will still be normal. Over time the pulmonary pressure will continue to rise and eventually severe Pulmonary Arterial Hypertension develops.
Heart Murmur
Many patients who have an ASD will have a murmur in their heart. This murmur or symptoms of shortness of breath eventually lead to an echocardiogram. This ultrasound study generally will show the enlarged right side of the heart and increased pulmonary artery pressures. Depending on the location and size of the hole, it may even be visible on the echocardiogram.
Heart Catheterization and Other PAH Tests
A heart catheterization and exercise testing along with the usual battery of PAH tests (blood work, chest Xray, and breathing tests) are performed. The heart catheterization is the most important test to determine if the hole in the heart should be closed. Occasionally an MRI of the heart is helpful as well. If there is evidence of a large hole and the pulmonary hypertension is only mild, then the hole is usually closed. If the PAH is severe then we generally avoid closing the hole.
Closure of an Atrial Septal Defect
Closure of an ASD can be done via a catheter-based procedure (through your groin using a long tube) or by an open-heart procedure. When possible, the catheter-based procedure is always preferred. Some holes are so large that only a surgery can fix the problem.
Development of PAH
Some patients who have had their ASD closed may develop PAH several years later. This could be due to lack of adequate testing to identify PAH prior to closure or PAH may simply develop a few years later. When this happens we treat the PAH with our usual medications. Prior to closing an ASD it is very important to carefully evaluate for PAH. This is because a hole in the heart can actually be helpful once PAH develops.
Most patients with an ASD will never develop PAH. However, if you have been diagnosed with an ASD, you should be carefully evaluated for this problem. Either a PAH expert or an expert in congenital heart disease can help quarterback this evaluation.
